Childhood trauma
Childhood trauma is often described as serious adverse childhood experiences (ACEs).[1] Children may go through a range of experiences that classify as psychological trauma, these might include neglect,[2] abandonment,[2] sexual abuse, and physical abuse,[2] witnessing abuse of a sibling or parent, or having a mentally ill parent. These events have profound psychological, physiological, and sociological impacts and can have negative, lasting effects on health and well-being. Kaiser Permanente and the Centers for Disease Control and Prevention's 1998 study on adverse childhood experiences determined that traumatic experiences during childhood are a root cause of many social, emotional, and cognitive impairments that lead to increased risk of unhealthy self-destructive behaviors,[2] risk of violence or re-victimization, chronic health conditions, low life potential and premature mortality. As the number of adverse experiences increases, the risk of problems from childhood through adulthood also rises.[3] Nearly 30 years of study following the initial study has confirmed this. Many states, health providers, and other groups now routinely screen parents and children for ACEs.
Health outcomes
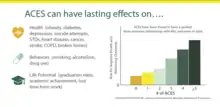
Traumatic experiences during childhood causes stress that increases an individual's allostatic load and thus affects the immune system, nervous system, and endocrine system.[4][5][6][7] Childhood trauma is often associated with adverse health outcomes including depression, hypertension, autoimmune diseases, lung cancer, and premature mortality.[4][6][8][9] Effects of childhood trauma on brain development includes a negative impact on emotional regulation and impairment of development of social skills.[6] Research has shown that children raised in traumatic or risky family environments tend to have excessive internalizing (e.g., social withdrawal, anxiety) or externalizing (e.g., aggressive behavior), and suicidal behavior.[6][10][11] Recent research has found that physical and sexual abuse are associated with mood and anxiety disorders in adulthood, while personality disorders and schizophrenia are linked with emotional abuse as adults.[12][13]
Psychological impact
Childhood trauma can increase the risk of mental disorders including posttraumatic stress disorder (PTSD), attachment issues, depression, and substance abuse. Sensitive and critical stages of child development can result in altered neurological functioning, adaptive to a malevolent environment but difficult for more benign environments.
In a study done by Stefania Tognin and Maria Calem comparing healthy comparisons (HC) and individuals at clinically high risk for developing psychosis (CHR), 65.6% CHR patients and 23.1% HC experienced some level of childhood trauma. The conclusion of the study shows that there is a correlation between the effects of childhood trauma and the being at high risk for psychosis.[14]
Epigenetics
Childhood trauma can leave epigenetic marks on a child's genes, which chemically modify gene expression by silencing or activating genes.[15] This can alter fundamental biological processes and adversely affect health outcomes throughout life.[15] A 2013 study found that people who had experienced childhood trauma had different neuropathology than people with PTSD from trauma experienced after childhood.[15] Another recent study in rhesus macaques showed that DNA methylation changes related to early-life adversity persisted into adulthood.[16]
The theoretical link between exposure to extreme stress and the development of PTSD provided the rationale for early hypotheses that PTSD-related biological alterations would be similar in direction to those observed acutely in animals exposed to stressors. When subsequent findings indicated that only a minority of trauma-exposed individuals develop PTSD, an alternative hypothesis was generated proposing that PTSD involves a failure of mechanisms involved in recovery and restitution of physiological homeostasis, possibly resulting from individualistic predisposition. Translational studies of PTSD are the use of a developmental neurobiological approach, spanning across the entire course of the illness. Symptom severity in PTSD can wax and wane over several decades. Biological alterations reflecting risk rather than pathophysiology may not account for this phenomenon. On the other hand, even putative risk factors such as glucocorticoid responsiveness and hippocampal volume show changes in response to factors such as environmental exposures, duration of illness, comorbidity, and aging. Thus, it is important to understand whether risk factors influence, or are influenced by, other parameters associated with PTSD (Yehuda, and LeDooux, 2007).[17]
In this sense parental trauma exposure is associated with greater risk for post-traumatic stress disorder (PTSD) and mood and anxiety disorders in offspring since biological alterations associated with PTSD and/or other stress-related disorders have also been observed in offspring of trauma survivors who do not themselves report trauma exposure or psychiatric disorder. Animal models have demonstrated that stress exposure can result in epigenetic alterations in the next generation, and such mechanisms have been hypothesized to underpin vulnerability to symptoms in offspring of trauma survivors. Enduring behavioral responses to stress and epigenetic alterations in adult offspring have been demonstrated to be mediated by changes in gametes in utero effects, variations in early postnatal care, and/or other early life experiences that are influenced by parental exposure (Yehuda, Daskalakis, Bierer, Bader, Klengel, Holsboer, and Binder, 2015).
Survivors of war trauma or childhood maltreatment are at increased risk for trauma-spectrum disorders[18] such as post-traumatic stress disorder (PTSD). In addition, traumatic stress has been associated with alterations in the neuroendocrine and the immune system, enhancing the risk for physical diseases. Traumatic experiences might even affect psychological as well as biological parameters in the next generation, i.e. traumatic stress might have trans generational effects.[18] So currently there is a new field trying to explain how epigenetic processes, which represent a pivotal biological mechanism for dynamic adaptation to environmental challenges, might contribute to the explanation of the long-lasting and intergenerational effects of trauma.[18] In particular, epigenetic alterations in genes regulating the hypothalamus–pituitary–adrenal axis as well as the immune system have been observed in survivors of childhood and adult trauma.[19]
These changes could result in enduring alterations of the stress response as well as the physical health risk. Furthermore, the effects of parental trauma could be transmitted to the next generation by parental distress and the pre- and postnatal environment, as well as by epigenetic marks transmitted via the germline. While epigenetic research has a high potential of advancing our understanding of the consequences of trauma, the findings have to be interpreted with caution, as epigenetics only represent one piece of a complex puzzle of interacting biological and environmental factors.[18]
The mechanism of intergenerational transmission of epigenetic effects at bin 3/site 6 is not known but does not appear to be mediated by childhood adversity, as is the case for bin 2. From a biological perspective, accommodation to multiple environmental influences at distinct and potentially redundant sites on genes central to stress regulation would facilitate maximal stress responsively and adaptation.
Future studies should focus on assessing the effects of trauma at various developmental stages, as well as potential differences in maternal and paternal effects. Additionally, the mechanism of intergenerational transmission of trauma and functional importance of site specificity remain to be explored. Early detection of such epigenetic marks may advance the development of preventive strategies to address the intergenerational sequel of exposure to trauma.
As it has been said Cytosine methylation of glucocorticoid related genes represents an epigenetic modification thought to underlie the developmental programming of hypothalamic-pituitary-adrenal (HPA) axis function.[19] The importance of epigenetic studies offer promise as diagnostic or prognostic markers, but it is not known whether these measures associate with, or predict, clinical state.
Subsequent studies in humans showed that childhood adversity associates with higher methylation of the GR exon 1F promoter (the human ortholog of the rat exon 17 promoter sequence) lower hippocampal GR expression and increased HPA-axis responses to stress. The examination of biological measures in association with PTSD symptom change following an efficacious psychotherapy trial was designed to yield a sample with a variable degree of symptom improvement, with some showing large decreases in symptom severity, and others, minimal or moderate change. An additional advantage of this approach is the ability to modify symptoms without introducing exogenousmedications that might have direct effects on the biological measures of interest. (Yehuda, Daskalakis, Desarnaud, Makotkine, Lehrner, Koch, Flory, Buxbaum, Meaney, and Bierer, 2013; Yahyavi, Zarghami, Marwah, 2014).
Epidemiologic research has clarified risk factors that increase the likelihood of PTSD after exposure to a potentially traumatic event. PTSD is an interaction between a subject, a traumatogenic factor and a social context. With each epidemiological, psychopathological and more particularly neurogenetic study, we will expand on the impact of these interactions on the therapeutic treatment of psycho-traumatized persons (Uuxéméry, 2012).
Reference
- Zhao, Roseanne. "Child Abuse Leaves Epigenetic Marks". National Human Genome Research Institute.
- Xiong, Fuxia; Zhang, Lubo (January 2013). "Role of the hypothalamic–pituitary–adrenal axis in developmental programming of health and disease". Frontiers in Neuroendocrinology. 34 (1): 27–46. doi:10.1016/j.yfrne.2012.11.002. PMC 3594480. PMID 23200813.
Socioeconomic costs
The social and economic costs of child abuse and neglect are difficult to calculate. Some costs are straightforward and directly related to maltreatment, such as hospital costs for medical treatment of injuries sustained as a result of physical abuse and foster care costs resulting from the removal of children when they cannot remain safely with their families. Other costs, less directly tied to the incidence of abuse, include lower academic achievement, adult criminality, and lifelong mental health problems. Both direct and indirect costs impact society and the economy.[20][21]
Transgenerational effects
People can pass their epigenetic marks including de-myelinated neurons to their children. The effects of trauma can be transferred from one generation of childhood trauma survivors to subsequent generations of offspring. This is known as transgenerational trauma or intergenerational trauma, and can manifest in parenting behaviors as well as epigenetically.[22][23][24] Exposure to childhood trauma, along with environmental stress, can also cause alterations in genes and gene expressions.[25][26][27] A growing body of literature suggests that children's experiences of trauma and abuse within close relationships not only jeopardize their well-being in childhood, but can also have long-lasting consequences that extend well into adulthood.[28] These long-lasting consequences can include emotion regulation issues, which can then be passed onto subsequent generations through child-parent interactions and learned behaviors.[29] (see also behavioral epigenetics, epigenetics, historical trauma, and cycle of violence)
Resilience
Exposure to maltreatment in childhood significantly predicts a variety of negative outcomes in adulthood.[30] However, not all children who are exposed to a potentially traumatic event develop subsequent struggles with mental or physical health.[31] Therefore, there are factors that reduce the impact of potentially traumatic events and protect an individual from developing mental health problems after exposure to a potentially traumatic event. These are called resiliency factors.
Research regarding children who showed adaptive development while facing adversity began in the 1970s and continues to this day.[32] Resilience is defined as “the process of, capacity for, or outcome of successful adaptation despite challenging or threatening circumstances."[33] The concept of resilience stems from research that showed experiencing positive emotions had a restorative and preventive effect on the experience of negative emotions more broadly with regards to physical and psychological wellbeing in general and more specifically with reactions to trauma.[34][35] This line of research has contributed to the development of interventions that focus on promoting resilience as opposed to focusing on deficits in an individual who has experienced a traumatic event.[32] Resilience has been found to decrease risk of suicide, depression, anxiety and other mental health struggles associated with exposure to trauma in childhood.[36][37][38][39]
When an individual who is high in resilience experiences a potentially traumatic event, their relative level of functioning does not significantly deviate from the level of functioning they exhibited prior to exposure to a potentially traumatic event.[33] Furthermore, that same individual may recover more quickly and successfully from a potentially traumatic experience than an individual who could be said to be less resilient.[33] In children, level of functioning is operationalized as the child continuing to behave in a manner that is considered developmentally appropriate for a child of that age.[32] Level of functioning is also measured by the presence of mental health disorders such as depression, anxiety, posttraumatic stress disorder, and so on.[31]
Factors that affect resilience
Factors that affect resilience include cultural factors like socioeconomic status, such that having more resources at one's disposal usually equates to more resilience to trauma.[32] Furthermore, the severity and duration of the potentially traumatic experience affect the likelihood of experiencing negative outcomes as a result of childhood trauma.[31][37] One factor that does not affect resilience is gender, with both males and females being equally sensitive to risk and protective factors.[31] Cognitive ability is also not a predictor of resilience.[31]
Attachment has been shown to be one of the most important factors to consider when it comes to evaluating the relative resilience of an individual.[31] Children with secure attachments to an adult with effective coping strategies were most likely to endure adverse childhood experiences (ACEs) in an adaptive manner.[32] Secure attachments throughout the lifespan (including in adolescence and adulthood) appear to be equally important in fostering and maintaining resilience.[31] Secure attachment to one's peers throughout adolescence is a particularly strong predictor of resilience.[31] Within the context of abuse, it is thought that these secure attachments decrease the extent to which children who are abused perceive others as being untrustworthy.[31] In other words, while some children who are abused might begin to view other people as being unsafe and unable to be trusted, children who are able to develop and maintain healthy relationships are less likely to hold these views. Children who experience trauma but also experience healthy attachment with multiple groups of people (in essence, adults, peers, romantic partners, etc.) throughout childhood, adolescence, and adulthood are particularly resilient.[31]
Personality also affects the development (or lack of development) of adult psychopathology as a result of childhood abuse.[31] Individuals who scored low in neuroticism exhibit fewer negative outcomes, such as psychopathology, criminal activity, and poor physical health, after exposure to a potentially traumatic event.[31] Furthermore, individuals with higher scores on openness to experience, conscientiousness, and extraversion have been found to be more resilient to the effects of childhood trauma.[40][41]
Enhancing resilience
One of the most common misconceptions about resilience is that individuals who show resilience are somehow special or extraordinary in some way.[32] Successful adaptation, or resilience, is quite common among children.[32] This is due in part to the naturally adaptive nature of childhood development. Therefore, resilience is enhanced by protecting against factors that might undermine a child's inborn resilience.[32] Studies suggest that resiliency can be enhanced by providing children who have been exposed to trauma with environments in which they feel safe and are able to securely attach to a healthy adult.[42] Therefore, interventions that promote strong parent-child bonds are particularly effective at buffering against the potential negative effects of trauma.[42]
Furthermore, researchers of resilience argue that successful adaptation is not merely an end result but rather a developmental process that is ongoing throughout a person's lifetime.[42] Thus, successful promotion of resilience must also be ongoing throughout a person's lifespan.
Prognosis
Trauma affects all children differently (see stress in early childhood). Some children who experience trauma develop significant and long-lasting problems, while others may have minimal symptoms and recover more quickly.[43] Studies have found that despite the broad impacts of trauma, children can and do recover, and that trauma-informed care and interventions produce better outcomes than “treatment as usual”. Trauma-informed care is defined as offering services or support in a way that addresses the special needs of people who have experienced trauma.[44]
Types of trauma
Bullying
Bullying is any unprovoked action with the intention of harming, either physically or psychologically, someone who is considered to have less power, either physically or socially. Bullying is a form of harassment that is often repeated and habitual, and can happen in person or online.[45]
Bullying in childhood may inflict harm or distress and educational harm that can affect the later stage of adolescence.[46] Bullying involvement, as victim, bully, bully/victim, or witness, can threaten the well-being of children. Bullying can be a risk factor for the development of an eating disorder, it can impact the functioning of the HPA axis, and it can impact functioning in adulthood. It increases the risk for physical problems such as inflammation, diabetes, and heart risk, and mental health problems such as anxiety, depression, agoraphobia, panic disorder, substance abuse, and PTSD.[47]
Community violence
Unlike bullying which is direct, trauma from community violence is not always directly perpetuated on the child, but is instead the result of being exposed to violent acts and behaviors in the community, such as gang violence, school shootings, riots, or police brutality.[48] Community violence exposure whether direct, or indirect, is associated with many negative mental health outcomes among children and adolescents including internalizing trauma-related symptoms,[49] academic problems,[50] substance abuse,[51] and suicidal ideation.[52]
Evidence also indicates that violence tends to beget more violence; children who witness community violence consistently show higher levels of aggression across developmental periods including early[49] and middle childhood,[53][54] as well as adolescence.[55]
Complex trauma
Complex trauma occurs from exposure to multiple and repetitive episodes of victimization or other traumatic events. Individuals who are exposed to multiple forms of trauma often display a wide range of difficulties compared to those who have only had one of few trauma exposures. For example, cognitive complications (dissociation), affective, somatic, behavioral, relational, and self-attributional problems have been seen in individuals who have experienced complex trauma.[56]
Disasters
Beyond the experience of natural and man-made disasters themselves, disaster-related traumas include the loss of loved ones, disruptions caused by disaster-caused homelessness and hardship and the breakdown of community structures.[57]
Exposure to a natural disaster is a highly stressful experiences that can lead to a wide range of maladaptive outcomes, particularly in children.[58] Exposure to natural disaster constitutes a risk factor for poor psychological health in children and adolescents. Psychological symptoms tend to decline over time after the exposure, it is not a rapid process.[59]
Intimate partner violence
Similar to community violence, intimated partner violence-related trauma is not necessarily directly perpetuated on child, but can be the result of exposure to violence within the household, often of violence perpetuated against one or more caregivers or family members. It is often accompanied by direct physical and emotional abuse of the child.[60] Witnessing violence and threats against a caregiver during early years of life is associated with severe impacts on a child's health and development.
Outcomes for children include psychological distress, behavioral disorders, disturbances in self-regulation, difficulties with social interaction, and disorganized attachment.[61] The impact of seeing intimate partner violence could be more serious for younger children. Younger children are completely dependent on their caregivers than older children not only for physical care but also emotional care. This is needed for them to develop normal neurological, psychological, and social development. This dependence can contribute to their vulnerability to witnessing violence against their caregivers.
Medical trauma
Medical trauma, sometimes called 'paediatric medical traumatic stress' refers to a set of psychological and physiological responses of children and their families to pain, injury, serious illness, medical procedures, and invasive or frightening treatment experiences. Medical trauma may occur as a response to a single or multiple medical events.[62] In children, they are still developing cognitive skills and because of this they process information differently. They might associate pain with punishment and could believe they did something wrong that led to them being in pain or that they somehow caused their injury.[63]
Children may experience disruptions in their attachment with their caregivers due to their traumatic medical experience. This does depend on the age of the child and their understanding of their medical difficulties. For example, a young child may feel betrayed by their parents if they have had to participate in activities that have cause and contributed to the child's pain such as administering medications or taking them to the doctor. At the same time, the parent-child relationship is strained due to parents feeling powerless, guilt, or inadequacy.[63]
Physical abuse
Child physical abuse is physical trauma or physical injury caused by slapping, beating, hitting, or otherwise harming a child.[64] This abuse is considered non-accidental. Injuries can range from mild bruising to broken bones, skull fractures, and even death.[65] Short term consequences of physical abuse of children include fractures,[66] cognitive or intellectual disabilities, social skills deficits, PTSD, other psychiatric disorders,[65] heightened aggression, and externalizing behaviors,[67] anxiety, risk-taking behavior, and suicidal behavior.[68] Long-term consequences include difficulty trusting others, low self-esteem, anxiety, physical problems, anger, internalization of aggression, depression, interpersonal difficulties, and substance abuse.
Refugee trauma
Refugee-related childhood trauma can take place in the child's country of origin due to war, persecution, or violence, but can also be a result of the process of displacement or even the disruptions and transitions of resettlement into the destination country.[69] Studies of refugee youth report high levels of exposure to war related trauma and have found profound averse consequences of these experiences for children's mental health. Some outcomes from experiencing trauma in refugee children are behavioral problems, mood and anxiety disorders, PTSD, and adjustment difficulty.[70]
Separation trauma
Separation trauma[71] is a disruption in an attachment relationship that disrupts neurological development and can lead to death.[72][73] Chronic separation from a caregiver can be extremely traumatic to a child.[74][75]
Sexual abuse
Traumatic grief
Traumatic grief is distinguished from the traditional grieving process in that the child is unable to cope with daily life, or even remember a loved one outside of the circumstances of their death. This can often be the case when the death is the result of a sudden illness or an act of violence.[76]
Treatment
The effects of childhood trauma can be mitigated through care and treatment. Early intervention has significant impact.[77][78] Sometimes support and nurturing from caregivers or other family members is enough to avoid long term harm; but in cases where children need professional care, trauma focused therapies will be used.[79] Trauma-informed treatment modalities treat the whole person, recognizing the impact of trauma on physical, psychological, and social health.[80]
Reducing stress hormones (cortisol, adrenaline, testosterone) is a vital early step for effective treatment of complex childhood trauma.[81]
Cognitive behavioral therapy (CBT) is the psychological treatment of choice for PTSD and is recommended by best-practice treatment guidelines e.g. CBT typically involves confrontation with, and processing of, the trauma memory in a safe, gradual manner; identification and restructuring of problematic beliefs; and de-arousal skills. There is strong research evidence for use of these CBT techniques to treat PTSD in terms of magnitude of symptom reduction from pre-treatment levels, and diagnostic recovery. Associated treatment barriers include stigma, cost, geography and insufficient treatment availability.[82]
Dialectical Behavior Therapy (DBT) has been shown to be help prevent self-harm and enhance interpersonal functioning by reducing experiential avoidance and expressed anger through a combination of cognitive behavioral and mindfulness techniques.[83]
The Real Life Heroes (RLH) treatment, a sequential, attachment-centered treatment intervention for children with Complex PTSD that focuses on 3 primary components: affect regulation, emotionally supportive relationships, and life story integration to build resources and skills for resilience.
The Narrative-Emotion Process Coding System (NEPCS) is a behavioral coding system that identifies eight client markers: Abstract Story, Empty Story, Unstoried Emotion, Inchoate Story, Same Old Story, Competing Plotlines Story, Unexpected Outcome Story, and Discovery Story. Each marker varies in the degree to which specific narrative and emotion process indicators are represented in one-minute time segments drawn from videotaped therapy sessions. As enhanced integration of narrative and emotional expression has previously been associated with recovery from complex trauma.[84]
The Attachment, Self-Regulation, and Competency (ARC) Framework is an intervention for children and adolescents impacted by complex trauma. The ARC framework is a flexible, component-based intervention for treating children and adolescents who have experienced complex trauma. Theoretically grounded in attachment, trauma, and developmental theories and specifically addresses three core domains impacted by exposure to chronic, interpersonal trauma: attachment, self-regulation, and developmental competencies Attachment, self -regulation, competency, trauma experience integration, within those domains, the framework is organized around 10 core targets or building blocks of intervention.[85]
Effects on adults
As an adult feelings of anxiety, worry, shame, guilt, helplessness, hopelessness, grief, sadness and anger that started with a trauma in childhood can continue. In addition, those who endure trauma as a child are more likely to encounter anxiety, depression, suicide and self harm, PTSD, drug and alcohol misuse and relationship difficulties.[86] The effects of childhood trauma don't end with just emotional repercussions. Survivors of childhood trauma are also at higher risk of developing asthma, coronary heart disease, diabetes or having a stroke. They are also more likely to develop a "heightened stress response" which can make it difficult for them to regulate their emotions, lead to sleep difficulties, lower immune function, and increase the risk of a number of physical illnesses throughout adulthood.[86]
References
- Pearce, J; Murray, C; Larkin, W (July 2019). "Childhood adversity and trauma: experiences of professionals trained to routinely enquire about childhood adversity". Heliyon. 5 (7): e01900. doi:10.1016/j.heliyon.2019.e01900. PMC 6658729. PMID 31372522.
- Van Der Kolk, B. A.; Perry, J. C.; Herman, J. L. (1992). "Childhood origins of self-destructive behavior". American Journal of Psychiatry. 12 (148): 1665–71. doi:10.1176/ajp.148.12.1665. PMID 1957928.
- "The Adverse Childhood Experiences (ACE) Study". Centers for Diesase Control. Retrieved 6 June 2017.
- Brown DW, Anda RF, Felitti VJ, Edwards VJ, Malarcher AM, Croft JB, Giles WH (January 2010). "Adverse childhood experiences are associated with the risk of lung cancer: a prospective cohort study". BMC Public Health. 10: 20. doi:10.1186/1471-2458-10-20. PMC 2826284. PMID 20085623.
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB (February 2009). "Cumulative childhood stress and autoimmune diseases in adults". Psychosomatic Medicine. 71 (2): 243–50. doi:10.1097/PSY.0b013e3181907888. PMC 3318917. PMID 19188532.
- Taylor SE, Lerner JS, Sage RM, Lehman BJ, Seeman TE (December 2004). "Early environment, emotions, responses to stress, and health". Journal of Personality. 72 (6): 1365–93. CiteSeerX 10.1.1.324.5195. doi:10.1111/j.1467-6494.2004.00300.x. PMID 15509286.
- Motzer SA, Hertig V (March 2004). "Stress, stress response, and health". The Nursing Clinics of North America. 39 (1): 1–17. doi:10.1016/j.cnur.2003.11.001. PMID 15062724.
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF (October 2004). "Adverse childhood experiences and the risk of depressive disorders in adulthood". Journal of Affective Disorders. 82 (2): 217–25. doi:10.1016/j.jad.2003.12.013. PMID 15488250.
- Murphy MO, Cohn DM, Loria AS (March 2017). "Developmental origins of cardiovascular disease: Impact of early life stress in humans and rodents". Neuroscience and Biobehavioral Reviews. 74 (Pt B): 453–465. doi:10.1016/j.neubiorev.2016.07.018. PMC 5250589. PMID 27450581.
- Aron EN, Aron A, Davies KM (February 2005). "Adult shyness: the interaction of temperamental sensitivity and an adverse childhood environment". Personality & Social Psychology Bulletin. 31 (2): 181–97. doi:10.1177/0146167204271419. PMID 15619591. S2CID 1679620.
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T (2012). "The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis". PLOS Medicine. 9 (11): e1001349. doi:10.1371/journal.pmed.1001349. PMC 3507962. PMID 23209385.
- Sachs-Ericsson NJ, Sheffler JL, Stanley IH, Piazza JR, Preacher KJ (October 2017). "When Emotional Pain Becomes Physical: Adverse Childhood Experiences, Pain, and the Role of Mood and Anxiety Disorders". Journal of Clinical Psychology. 73 (10): 1403–1428. doi:10.1002/jclp.22444. PMC 6098699. PMID 28328011.
- Carr CP, Martins CM, Stingel AM, Lemgruber VB, Juruena MF (December 2013). "The role of early life stress in adult psychiatric disorders: a systematic review according to childhood trauma subtypes". The Journal of Nervous and Mental Disease. 201 (12): 1007–20. doi:10.1097/NMD.0000000000000049. PMID 24284634. S2CID 205878806.
- Tognin, Stefania; Calem, Maria (1 March 2017). "M122. Impact of Childhood Trauma on Educational Achievement in Young People at Clinical High Risk of Psychosis". Schizophrenia Bulletin. 43 (suppl_1): S255. doi:10.1093/schbul/sbx022.116. PMC 5475870.
- Mehta, Divya; Klengel, Torsten; Conneely, Karen N.; Smith, Alicia K.; Altmann, André; Pace, Thaddeus W.; Rex-Haffner, Monika; Loeschner, Anne; Gonik, Mariya; Mercer, Kristina B.; Bradley, Bekh; Müller-Myhsok, Bertram; Ressler, Kerry J.; Binder, Elisabeth B. (14 May 2013). "Childhood maltreatment is associated with distinct genomic and epigenetic profiles in posttraumatic stress disorder". Proceedings of the National Academy of Sciences of the United States of America. 110 (20): 8302–8307. Bibcode:2013PNAS..110.8302M. doi:10.1073/pnas.1217750110. PMC 3657772. PMID 23630272. Lay summary.
- Provençal N, Suderman MJ, Guillemin C, Massart R, Ruggiero A, Wang D, et al. (October 2012). "The signature of maternal rearing in the methylome in rhesus macaque prefrontal cortex and T cells". The Journal of Neuroscience. 32 (44): 15626–42. doi:10.1523/JNEUROSCI.1470-12.2012. PMC 3490439. PMID 23115197.
- Yehuda, Rachel; LeDoux, Joseph (October 2007). "Response Variation following Trauma: A Translational Neuroscience Approach to Understanding PTSD". Neuron. 56 (1): 19–32. doi:10.1016/j.neuron.2007.09.006. PMID 17920012. S2CID 25239428.
- Ramo-Fernández, Laura; Schneider, Anna; Wilker, Sarah; Kolassa, Iris-Tatjana (October 2015). "Epigenetic Alterations Associated with War Trauma and Childhood Maltreatment: Epigenetics of trauma and violence". Behavioral Sciences & the Law. 33 (5): 701–721. doi:10.1002/bsl.2200. PMID 26358541.
- Xiong, Fuxia; Zhang, Lubo (January 2013). "Role of the hypothalamic–pituitary–adrenal axis in developmental programming of health and disease". Frontiers in Neuroendocrinology. 34 (1): 27–46. doi:10.1016/j.yfrne.2012.11.002. PMC 3594480. PMID 23200813.
- "Social and Economic Consequences of Child Abuse and Neglect". Child Welfare Information Gateway. U.S. Department of Health and Human Services.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "The Estimated Annual Cost of Child Abuse and Neglect". Prevent Child Abuse America.
- Fox M (2 May 2016). "Poor Parenting Can Be Passed From Generation to Generation". NBC News. Retrieved 2017-03-16.
- "Childhood trauma compromises health via diverse pathways". The Blue Knot Foundation. Archived from the original on 2017-03-22. Retrieved 2017-03-16.
- "Adverse Childhood Experiences (ACEs): Mental Illness of a Parent". Crow Wing Energized. Archived from the original on 2017-03-22. Retrieved 2017-03-16.
- Roth TL (November 2013). "Epigenetic mechanisms in the development of behavior: advances, challenges, and future promises of a new field". Development and Psychopathology. 25 (4 Pt 2): 1279–91. doi:10.1017/S0954579413000618. PMC 4080409. PMID 24342840.
- Feder A, Nestler EJ, Charney DS (June 2009). "Psychobiology and molecular genetics of resilience". Nature Reviews. Neuroscience. 10 (6): 446–57. doi:10.1038/nrn2649. PMC 2833107. PMID 19455174.
- Tyrka AR, Ridout KK, Parade SH (November 2016). "Childhood adversity and epigenetic regulation of glucocorticoid signaling genes: Associations in children and adults". Development and Psychopathology. 28 (4pt2): 1319–1331. doi:10.1017/S0954579416000870. PMC 5330387. PMID 27691985.
- Kaplan SJ, Pelcovitz D, Labruna V (October 1999). "Child and adolescent abuse and neglect research: a review of the past 10 years. Part I: Physical and emotional abuse and neglect". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (10): 1214–22. doi:10.1097/00004583-199910000-00009. PMID 10517053.
- Juul, Sarah H.; Hendrix, Cassandra; Robinson, Brittany; Stowe, Zachary N.; Newport, D. Jeffrey; Brennan, Patricia A.; Johnson, Katrina C. (1 February 2016). "Maternal early-life trauma and affective parenting style: the mediating role of HPA-axis function". Archives of Women's Mental Health. 19 (1): 17–23. doi:10.1007/s00737-015-0528-x. PMID 25956587. S2CID 11124814.
- Arnow, B. A. (2004). "Relationships between childhood maltreatment, adult health and psychiatric outcomes, and medical utilization". Journal of Clinical Psychiatry. 65: 10–15.
- Collishaw, Stephan; Pickles, Andrew; Messer, Julie; Rutter, Michael; Shearer, Christina; Maughan, Barbara (March 2007). "Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample". Child Abuse & Neglect. 31 (3): 211–229. doi:10.1016/j.chiabu.2007.02.004. PMID 17399786.
- Masten, Ann S. (2001). "Ordinary magic: Resilience processes in development". American Psychologist. 56 (3): 227–238. doi:10.1037//0003-066x.56.3.227. PMID 11315249.
- Masten, Ann S.; Best, Karin M.; Garmezy, Norman (October 1990). "Resilience and development: Contributions from the study of children who overcome adversity". Development and Psychopathology. 2 (4): 425–444. doi:10.1017/S0954579400005812.
- "Cultivating positive emotions to optimize health and well-being". Prevention & Treatment. 3: np. 2000. CiteSeerX 10.1.1.194.4228. doi:10.1037//1522-3736.3.0001a.
- Tugade, Michele M.; Fredrickson, Barbara L.; Feldman Barrett, Lisa (December 2004). "Psychological Resilience and Positive Emotional Granularity: Examining the Benefits of Positive Emotions on Coping and Health". Journal of Personality. 72 (6): 1161–1190. doi:10.1111/j.1467-6494.2004.00294.x. PMC 1201429. PMID 15509280.
- Roy, Alec; Carli, Vladimir; Sarchiapone, Marco (October 2011). "Resilience mitigates the suicide risk associated with childhood trauma". Journal of Affective Disorders. 133 (3): 591–594. doi:10.1016/j.jad.2011.05.006. PMID 21621850.
- Wingo, Aliza P.; Wrenn, Glenda; Pelletier, Tiffany; Gutman, Alisa R.; Bradley, Bekh; Ressler, Kerry J. (November 2010). "Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure". Journal of Affective Disorders. 126 (3): 411–414. doi:10.1016/j.jad.2010.04.009. PMC 3606050. PMID 20488545.
- Poole, Julia C.; Dobson, Keith S.; Pusch, Dennis (February 2017). "Childhood adversity and adult depression: The protective role of psychological resilience". Child Abuse & Neglect. 64: 89–100. doi:10.1016/j.chiabu.2016.12.012. PMID 28056359.
- Poole, Julia C.; Dobson, Keith S.; Pusch, Dennis (August 2017). "Anxiety among adults with a history of childhood adversity: Psychological resilience moderates the indirect effect of emotion dysregulation". Journal of Affective Disorders. 217: 144–152. doi:10.1016/j.jad.2017.03.047. PMID 28410477.
- Watson, David; Hubbard, Brock (December 1996). "Adaptational Style and Dispositional Structure: Coping in the Context of the Five-Factor Model". Journal of Personality. 64 (4): 737–774. doi:10.1111/j.1467-6494.1996.tb00943.x.
- Campbell-Sills, Laura; Cohan, Sharon L.; Stein, Murray B. (April 2006). "Relationship of resilience to personality, coping, and psychiatric symptoms in young adults". Behaviour Research and Therapy. 44 (4): 585–599. doi:10.1016/j.brat.2005.05.001. PMID 15998508.
- Yates, Tuppett M.; Egeland, Byron; Sroufe, L. Alan (2003). "Rethinking Resilience: A Developmental Process Perspective". Resilience and Vulnerability. pp. 243–266. doi:10.1017/cbo9780511615788.012. ISBN 978-0-521-00161-8.
- "Chapter 3, Understanding the Impact of Trauma.". Trauma-Informed Care in Behavioral Health Services. Trauma-Informed Care in Behavioral Health Services (Treatment Improvement Protocol (TIP) Series. 57. Rockville (MD): Center for Substance Abuse Treatment (US). 2014.
- SAMHSA's Concept of Trauma and Guidance for a Trauma-Informed Approach. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2014.
- Peterson, Sarah (2018-03-26). "Bullying". The National Child Traumatic Stress Network. Retrieved 2020-10-26.
- deLara, Ellen W. (September 2019). "Consequences of Childhood Bullying on Mental Health and Relationships for Young Adults". Journal of Child and Family Studies. 28 (9): 2379–2389. doi:10.1007/s10826-018-1197-y. S2CID 149830204.
- Copeland, William E.; Wolke, Dieter; Angold, Adrian; Costello, E. Jane (1 April 2013). "Adult Psychiatric Outcomes of Bullying and Being Bullied by Peers in Childhood and Adolescence". JAMA Psychiatry. 70 (4): 419–26. doi:10.1001/jamapsychiatry.2013.504. PMC 3618584. PMID 23426798.
- Peterson, Sarah (2017-12-08). "Community Violence". The National Child Traumatic Stress Network. Retrieved 2020-10-26.
- Fowler, Patrick J.; Tompsett, Carolyn J.; Braciszewski, Jordan M.; Jacques-Tiura, Angela J.; Baltes, Boris B. (January 2009). "Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents". Development and Psychopathology. 21 (1): 227–259. doi:10.1017/S0954579409000145. PMID 19144232. S2CID 8075374.
- Busby, Danielle R.; Lambert, Sharon F.; Ialongo, Nicholas S. (February 2013). "Psychological Symptoms Linking Exposure to Community Violence and Academic Functioning in African American Adolescents". Journal of Youth and Adolescence. 42 (2): 250–262. doi:10.1007/s10964-012-9895-z. PMC 4865382. PMID 23277294.
- Vermeiren, R.; Schwab-Stone, M.; Deboutte, D.; Leckman, P. E.; Ruchkin, V. (1 March 2003). "Violence Exposure and Substance Use in Adolescents: Findings From Three Countries". Pediatrics. 111 (3): 535–540. doi:10.1542/peds.111.3.535. PMID 12612233.
- Lambert, Sharon F.; Copeland-Linder, Nikeea; Ialongo, Nicholas S. (October 2008). "Longitudinal Associations Between Community Violence Exposure and Suicidality". Journal of Adolescent Health. 43 (4): 380–386. doi:10.1016/j.jadohealth.2008.02.015. PMC 2605628. PMID 18809136.
- Guerra, Nancy G.; Rowell Huesmann, L.; Spindler, Anja (October 2003). "Community Violence Exposure, Social Cognition, and Aggression Among Urban Elementary School Children". Child Development. 74 (5): 1561–1576. doi:10.1111/1467-8624.00623. hdl:2027.42/83426. PMID 14552414.
- Schwartz, David; Proctor, Laura J. (2000). "Community violence exposure and children's social adjustment in the school peer group: The mediating roles of emotion regulation and social cognition". Journal of Consulting and Clinical Psychology. 68 (4): 670–683. doi:10.1037/0022-006x.68.4.670. PMID 10965642.
- Bradshaw, Catherine P.; Rodgers, Caryn R. R.; Ghandour, Lilian A.; Garbarino, James (September 2009). "Social–cognitive mediators of the association between community violence exposure and aggressive behavior". School Psychology Quarterly. 24 (3): 199–210. doi:10.1037/a0017362.
- Courtois, Christine A.; Gold, Steven N. (2009). "The need for inclusion of psychological trauma in the professional curriculum: A call to action". Psychological Trauma: Theory, Research, Practice, and Policy. 1 (1): 3–23. doi:10.1037/a0015224.
- Peterson, Sarah (2018-01-25). "Disasters". The National Child Traumatic Stress Network. Retrieved 2020-10-26.
- Hansel, Tonya Cross; Osofsky, Howard J.; Osofsky, Joy D.; Speier, Anthony H. (June 2019). "Katrina inspired disaster screenings and services: School-based trauma interventions". Traumatology. 25 (2): 133–141. doi:10.1037/trm0000178.
- Adebäck, Petra; Schulman, Abbe; Nilsson, Doris (2 January 2018). "Children exposed to a natural disaster: psychological consequences eight years after 2004 tsunami". Nordic Journal of Psychiatry. 72 (1): 75–81. doi:10.1080/08039488.2017.1382569. PMID 28990835. S2CID 3082066.
- oseldman (2017-10-30). "Intimate Partner Violence". The National Child Traumatic Stress Network. Retrieved 2020-10-26.
- Evans, Sarah E.; Davies, Corrie; DiLillo, David (March 2008). "Exposure to domestic violence: A meta-analysis of child and adolescent outcomes". Aggression and Violent Behavior. 13 (2): 131–140. doi:10.1016/j.avb.2008.02.005.
- Marsac ML, Kassam-Adams N, Delahanty DL, Widaman KF, Barakat LP (December 2014). "Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period". Clinical Child and Family Psychology Review. 17 (4): 399–411. doi:10.1007/s10567-014-0174-2. PMC 4319666. PMID 25217001.
- Locatelli, Margaret G. (January 2020). "Play therapy treatment of pediatric medical trauma: A retrospective case study of a preschool child". International Journal of Play Therapy. 29 (1): 33–42. doi:10.1037/pla0000109.
- "Supplemental Material for Differences in Childhood Physical Abuse Reporting and the Association Between CPA and Alcohol Use Disorder in European American and African American Women". Psychology of Addictive Behaviors: adb0000174.supp. 2016. doi:10.1037/adb0000174.supp.
- Kolko, David J. (2001). "Child Physical Abuse". In Myers, John E. B.; Berliner, Lucy; Briere, John; Hendrix, C. Terry; Reid, Theresa; Jenny, Carole (eds.). The APSAC Handbook on Child Maltreatment. SAGE Publications. pp. 21–50. ISBN 978-0-7619-1991-9.
- Hoskote, Aparna U.; Martin, Katherine; Hormbrey, Philip; Burns, E. Claire (November 2003). "Fractures in infants: one in four is non-accidental". Child Abuse Review. 12 (6): 384–391. doi:10.1002/car.806.
- Manly, Jody Todd; Kim, Jungmeen E.; Rogosch, Fred A.; Cicchetti, Dante (December 2001). "Dimensions of child maltreatment and children's adjustment: Contributions of developmental timing and subtype". Development and Psychopathology. 13 (4): 759–782. doi:10.1017/s0954579401004023. PMID 11771907. S2CID 28118238.
- Finzi, Ricky; Har-Even, Dov; Shnit, Dan; Weizman, Abraham (1 December 2002). "Psychosocial Characterization of Physically Abused Children from Low Socioeconomic Households in Comparison to Neglected and Nonmaltreated Children". Journal of Child and Family Studies. 11 (4): 441–453. doi:10.1023/A:1020983308496. S2CID 140273333.
- Peterson, Sarah (2018-01-25). "Refugee Trauma". The National Child Traumatic Stress Network. Retrieved 2020-10-26.
- Betancourt, Theresa S.; Newnham, Elizabeth A.; Layne, Christopher M.; Kim, Soeun; Steinberg, Alan M.; Ellis, Heidi; Birman, Dina (December 2012). "Trauma History and Psychopathology in War-Affected Refugee Children Referred for Trauma-Related Mental Health Services in the United States: Trauma and Psychopathology of Refugee Children". Journal of Traumatic Stress. 25 (6): 682–690. doi:10.1002/jts.21749. PMID 23225034.
- Charlier, Thomas (2010). "Symbolisierung früher Trennungstraumata und Neubildung von Repräsentanzen" [Symbolization of early separation traumas and the formation of new representations]. Psyche (in German). 64 (1): 1–33.
- Ward MJ, Lee SS, Lipper EG (2000). "Failure-to-thrive is associated with disorganized infant-mother attachment and unresolved maternal attachment". Infant Mental Health Journal. 21 (6): 428–442. doi:10.1002/1097-0355(200011/12)21:6<428::aid-imhj2>3.0.co;2-b.
- Muñoz-Hoyos A, Augustin-Morales MC, Ruíz-Cosano C, Molina-Carballo A, Fernández-García JM, Galdó-Munoz G (November 2001). "Institutional childcare and the affective deficiency syndrome: consequences on growth, nutrition and development". Early Human Development. 65 Suppl: S145–52. doi:10.1016/s0378-3782(01)00216-x. PMID 11755045.
- Cook A, Spinazzola J, Ford J, Lanktree C, Blaustein M, Cloitre M, DeRosa R, Hubbard R, Kagan R (2005-05-01). "Complex Trauma in Children and Adolescents". Psychiatric Annals. 35 (5): 390–398. doi:10.3928/00485713-20050501-05.
- Kinzie JD, Sack WH, Angell RH, Manson S, Rath B (1986). "The Psychiatric Effects of Massive Trauma on Cambodian Children: I. The Children". Journal of the American Academy of Child Psychiatry. 25 (3): 370–376. doi:10.1016/s0002-7138(09)60259-4.
- Peterson, Sarah (2018-01-25). "Traumatic Grief". The National Child Traumatic Stress Network. Retrieved 2020-10-26.
- McPherson, Lynne; Gatwiri, Kathomi; Tucci, Joe; Mitchell, Janise; Macnamara, Noel (November 2018). "A paradigm shift in responding to children who have experienced trauma: The Australian treatment and care for kids program". Children and Youth Services Review. 94: 525–534. doi:10.1016/j.childyouth.2018.08.031.
- Black, Melissa; Hitchcock, Caitlin; Bevan, Anna; Leary, Cliodhna O; Clarke, James; Elliott, Rachel; Watson, Peter; Lafortune, Louise; Rae, Sarah (2018-04-24). "The HARMONIC trial: Study protocol for a randomised controlled feasibility trial of Shaping Healthy Minds – a modular transdiagnostic intervention for mood, stress and anxiety disorders in adults". doi:10.31234/osf.io/fvc9a. Cite journal requires
|journal=(help) - "Childhood Trauma". Bridges to Recovery. Retrieved 2021-03-29.
- "Trauma-Informed Care | ATTC Network". attcnetwork.org. Retrieved 2019-01-10.
- "Corrigendum". Nordic Journal of Psychiatry. 71 (4): 324. 19 May 2017. doi:10.1080/08039488.2017.1301704.
- Allen, Adrian R.; Newby, Jill M.; Smith, Jessica; Andrews, Gavin (December 2015). "Internet-based cognitive behavioural therapy (iCBT) for posttraumatic stress disorder versus waitlist control: study protocol for a randomised controlled trial". Trials. 16 (1): 544. doi:10.1186/s13063-015-1059-5. PMC 4666048. PMID 26628268. S2CID 16947803.
- Curtois, Christine (2009). Treating complex traumatic stress disorders: An evidence-based guide. Guildford Press. ISBN 978-1462513390.
- Carpenter, Naomi; Angus, Lynne; Paivio, Sandra; Bryntwick, Emily (2 April 2016). "Narrative and emotion integration processes in emotion-focused therapy for complex trauma: an exploratory process-outcome analysis". Person-Centered & Experiential Psychotherapies. 15 (2): 67–94. doi:10.1080/14779757.2015.1132756. S2CID 147513703.
- Arnsten, Amy F.T.; Raskind, Murray A.; Taylor, Fletcher B.; Connor, Daniel F. (January 2015). "The effects of stress exposure on prefrontal cortex: Translating basic research into successful treatments for post-traumatic stress disorder". Neurobiology of Stress. 1: 89–99. doi:10.1016/j.ynstr.2014.10.002. PMC 4244027. PMID 25436222.
- "Effects of Childhood Trauma on Adults". International Society for Traumatic Stress Studies. Retrieved February 17, 2019.